Crohn's disease and ulcerative colitis: Diagnostic tests and biomarkers to monitor
Published Mar 8, 2021 • By Clémence Arnaud
Crohn's disease and ulcerative colitis are two conditions whose prevalence is increasing in the western world. Though the diagnostic process can be both complex and lengthy, research continues to improve the diagnosis and treatment of these diseases.
What is the difference between Crohn's disease and ulcerative colitis? What are the diagnostic methods for these two diseases?
We tell you everything in our article!

Chronic inflammatory bowel disease (IBD)
Crohn's disease and ulcerative colitis both fall under the umbrella term of inflammatory bowel disease (IBD). They are two disorders that progress in the form of flare-ups and in different ways depending on the individual.
Crohn's disease may affect only the small intestine, only the colon or both organs in a combined manner.
Ulcerative colitis, on the other hand, affects the colon as well as the rectum.
Diagnosing Crohn's and ulcerative colitis
There are no specific tests to detect these two diseases, so it is therefore necessary to analyze the symptoms described by the patient, to carry out a clinical examination and other tests.
For Crohn's disease, colonoscopy is a diagnostic technique that is often used. It consists of inserting a thin, flexible tube with a small camera through the anus to observe the walls of the ileum. It is carried out under general anesthesia and must be performed on an empty stomach with a completely emptied colon.
Ulcerative colitis is often diagnosed using sigmoidoscopy (or proctosigmoidoscopy). Unlike a colonoscopy, there is no need to fast and this examination is carried out under light anesthesia. The objective is to view the colon by inserting a tube with a small camera through the anus.
In both conditions, when patients are unable to undergo these examinations, an ultrasound or MRI scan can be carried out.
Evolution of Crohn's disease and ulcerative colitis
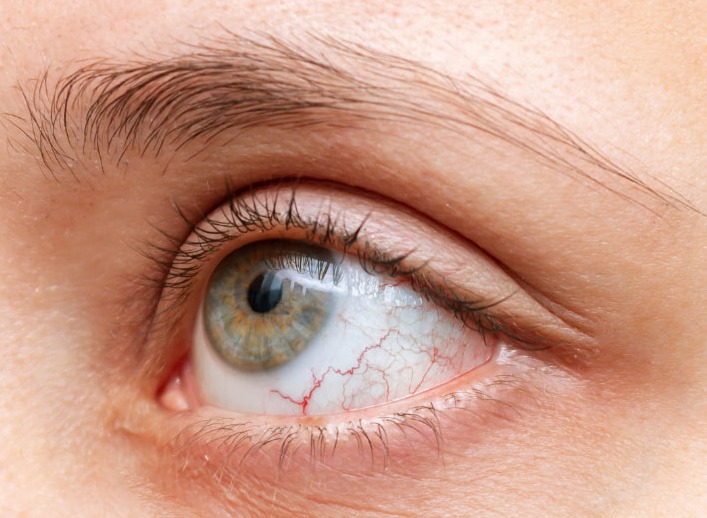
These two disorders cause persistent inflammation in the body. They can also lead to rheumatic problems including joint pain, eye problems (such as uveitis) or even vascular problems.
In the longer term, it is important to monitor for the risk of developing colon or intestinal cancer, thus requiring increased follow-up.
Biomarkers that can help lead to a diagnosis
Bacteriological and parasitological analysis of the stool can eliminate possible infection that may explain digestive symptoms.
Then, blood tests will look for signs of inflammation that can guide the diagnosis. Other factors such as C-reactive protein and erythrocyte sedimentation rate (ESR) are evaluated to determine the stage of the illness. These two parameters are determined by a blood test.
Anemia is also a commonly co-occurring condition in Crohn's and UC patients, as well as vitamin deficiencies. Anemia is a decrease in the total number of red blood cells in the blood. It can be linked to deficiencies such as iron deficiency. Indeed, in many chronic inflammatory conditions, the inflammatory response can interrupt the body's use of iron to produce red blood cells.
Fecal calprotectin level is another marker to be monitored. Typically, a 50 μg/g threshold of fecal calprotectin makes it possible to distinguish a functional disorder from an IBD-like disorder when digestive symptoms are not specific. During a flare-up, the threshold of 250 μg/g of fecal calprotectin is often exceeded, unlike when the disease is in remission.
Once the diagnosis has been made, it is important to evaluate the impacts that Crohn's disease and ulcerative colitis have on the kidneys, liver, nutritional balance, etc.
Research is ongoing
The Anterior gradient protein 2 homolog (AGR2) protein is widely studied in the inflammatory response of chronic conditions such as Crohn's disease or ulcerative colitis. This AGR2 protein could even play a precursory role in inflammatory bowel diseases.
The discovery of this protein is also an opportunity for new treatments to be developed, with the goal of targeting this protein and observing its effects.
>>> Feel free to read our article about blood understanding blood tests for IBD! <<<
Was this article helpful to you?
Share your thoughts and questions with the community in the comments below!
Take care!
Sources:
- Vidal - Maladie de Crohn
- Vidal - Rectocolite hémorragique
- Inflammatory bowel disease (IBD) - CDC
- How to get a diagnosis - Crohn's & Colitis UK
- Assurance maladie - Comment comprendre l'anémie ?
- INSERM - Maladie de Crohn : identification d'une protéine initiatrice de l'inflammation
- FMC gastro - Quand et comment utiliser la Calprotectine fécale au cours des MICI ?

 Facebook
Facebook Twitter
Twitter