Idiopathic inflammatory myopathy: symptoms, diagnosis and similarities with other diseases
Published Jan 17, 2022 • By Alizé Vives
Idiopathic inflammatory myopathy is a group of rare autoimmune diseases. They affect the skeletal striated muscles responsible for voluntary muscle contractions. The diagnosis of these diseases is usually based on a clinical examination during which the doctor examines the patient. In addition, other examinations may be carried out: electromyogram, biopsy, etc.
Because there exist different types of idiopathic inflammatory myopathy, it is important to differentiate between them in order to choose the most appropriate treatment which will ease the symptoms rapidly.
So what is idiopathic inflammatory myopathy? How is it diagnosed? How not to confuse it with other conditions?
We explain it all in our article!

What is idiopathic inflammatory myopathy?
This group of rare autoimmune diseases includes dermatomyositis, polymyositis, overlap myositis, inclusion body myositis, cancer-associated myositis and necrotizing autoimmune myopathy.
IMM affects about 6 to 7 people per 100,000. Women are diagnosed twice as often as men. The condition can occur at any age, but most often develops in adulthood.
The symptoms of IMM vary greatly, depending on the form, but can also differ from patient to patient, even if they are affected with the same form. Muscle damage occurs in the skeletal striated muscles that enable voluntary movement. Other dermatological, joint, muscle, lung and vascular manifestations may also be present.
The symptoms are caused by an unexplained reaction of the immune system which provokes inflammation. Genetic predisposition and environmental factors may be responsible for this disorder.
How can autoimmune inflammatory myopathy be diagnosed?
There are many diagnostic pitfalls. The physician should suspect IMM in the presence of the signs mentioned above, and the diagnosis should be confirmed by a specialist.
The diagnosis of autoimmune myositis is established after various examinations, including:
- Clinical examination, during which the doctor can identify the symptoms: skin rash (specific to dermatomyositis), joint pain, breathing difficulties, weight loss, fatigue, etc. The presence of one of these symptoms should lead to the search for other signs;
- Blood tests to detect the presence of autoantibodies (molecules produced by the immune system that target the muscles) that cause the symptoms. There are different types of autoantibodies, depending on the type of myositis. However, about 20% of patients have no identified autoantibodies;
- Muscle biopsy: this involves taking a sample of muscle tissue, in order to examine muscle cells under a microscope and look for abnormalities. Biopsy is a crucial element in the diagnosis of myositis because, in addition to its diagnostic value, it allows to confirm the type of myositis and can provide elements for prognosis. It is generally carried out by specialists who are familiar with every step of the procedure, such as, for example, taking a sufficient quantity of tissue, etc. The interpretation of the lesions requires a great deal of experience.
In order to establish the diagnosis, the doctor generally carries out a differential diagnosis. It is a method of differentiating a disease from other conditions that have similar symptoms or characteristics.
What are the conditions that should be differentiated from idiopathic inflammatory myopathy?
There are two main cases to consider when diagnosing idiopathic inflammatory myopathy: different types of inflammatory myositis and other conditions.
Different types of autoimmune inflammatory myositis
When diagnosing inflammatory myositis, it is important to define its type. Treatment is different for each type, and so is the management of the disease, given the diversity of symptoms and signs.
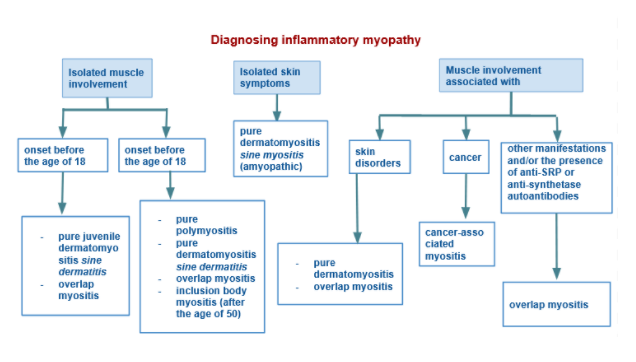
In the case of isolated muscle involvement and depending on the age of the patient at the time symptoms onset, different forms of inflammatory myositis can be evoked: dermatomyositis, overlap myositis, polymyositis or inclusion body myositis.
When skin involvement alone is observed, dermatomyositis is the only myositis that can be responsible.
In the case of muscle involvement associated with other symptoms, several types of myositis can be considered:
- In the presence of skin disorders, dermatomyositis or overlap myositis should be suggested;
- If cancer was diagnosed, the patient may develop cancer-associated myositis;
- In the case of other manifestations and/or the presence of anti-SRP or anti-synthetase autoantibodies, overlap myositis may be considered.
Other conditions
First of all, it is important to rule out any inflammatory myopathy caused by an external factor such as certain drugs (statins, etc.) or certain infectious agents.
It is also important to make a differential diagnosis with regard to other myopathies caused by nerve damage (peripheral neuropathy) or damage to the neuromuscular junction (the connection between the nerve supplying the information, and the muscle, such as myasthenia gravis).
When pulmonary symptoms (interstitial lung disease) are present in certain cases of dermatomyositis, other origins of myositis can be evoked (other than the autoimmune one), such as medicinal causes (more than 150 drugs have been identified), infectious ones (bacteria such as pneumococcus, haemophilus, legionella and mycoplasma, or viruses such as the influenza virus), environmental, specific and genetic origins.
In the presence of rheumatic symptoms such as myalgia, muscle edema detectable on the MRI and extra-muscular signs, myositis can be confused with other inflammatory rheumatic diseases such as polyarthritis or spondyloarthritis.
With regard to skin manifestations, some must be differentiated from those caused by other diseases:
- “Mechanics' hand”, thickened and cracked skin on the palm, frequently found in overlap myositis, may lead to confusion with similar conditions of allergic origin.
- Red eyelids, typical to dermatomyositis or overlap myositis, may also be present in much more common conditions such as contact dermatitis, atopic dermatitis, seborrhoeic dermatitis or rosacea.
- Gottron papules, plaques that are usually found on fingers, elbows or knees, can be confused with psoriasis.
- Redness on areas exposed to sunlight may mistakenly evoke lupus. However, in the case of lupus, these areas are located between the joints, whereas in the case of myositis, they are mostly located on the joints.
The diagnosis of idiopathic inflammatory myopathy requires an expert opinion from a neurologist, dermatologist and/or internist.
Was this article helpful to you?
Give it a like and share your thoughts and questions with the community in the comments below!
Take care !
Comments
You will also like

What are the dangers associated with the over-the-counter sale of certain medicines?
Dec 19, 2020 • 6 comments

 Facebook
Facebook Twitter
Twitter