Chronic Kidney Disease (CKD): Getting a Transplant and Best Practices after Surgery
Published Sep 18, 2023 • By Somya Pokharna
Our kidneys might very well be the unsung heroes of our body. However, conditions such as high blood pressure, diabetes, and infections can compromise their vital functions, significantly impacting an individual's quality of life.
What is chronic kidney disease? What causes it, and what are the symptoms? When is a transplant necessitated?
Discover all about it in this article!
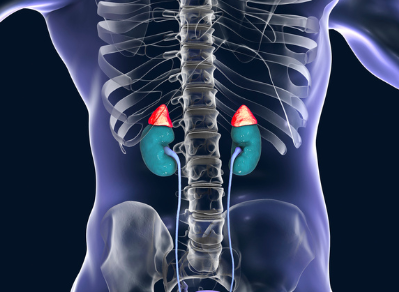
The kidneys are our body’s very own filtration system, cleaning all the blood coursing through it in just about half an hour. Not only do they work continuously to get rid of waste, toxins, and extra fluid, but they also help with releasing hormones to control blood pressure, generating more red blood cells, producing vitamin D to keep bones strong and healthy, and regulating the essential chemicals in our blood that we need to stay alive.
Unfortunately, however, up to 10% of the world's population, which is approximately 800 million people, gradually lose kidney function over time due to a condition known as chronic kidney disease.
What is chronic kidney disease?
Chronic kidney disease (CKD) is a condition in which the kidneys are damaged and can no longer perform vital functions like filtering the blood as well as they should, due to which waste and excess fluid remain in the body. This condition might then go on to cause other health problems, such as:
- Anemia or low count of red blood cells
- Edema, or swollen feet, hands, and ankles
- More frequent urination but decreased and discolored urine output
- Low calcium and high potassium and phosphorus levels in the blood, resulting in weakening of bones
- Hypertension, cardiovascular diseases, and stroke
- Weakened immune system and increased occurrence of infections.
- Loss of appetite
- Depression and fatigue
What causes chronic kidney disease?
CKD is typically the result of various underlying conditions that put a strain on the kidneys, such as:
- High blood pressure: Over time, this can stress the small blood vessels in the kidneys, impairing their proper function.
- Type 1 and Type 2 Diabetes: Elevated glucose levels in the blood can harm the tiny filters (glomeruli) within the kidneys.
- High cholesterol: This can lead to the accumulation of fatty deposits in the blood vessels that supply the kidneys, making it more challenging for them to function effectively.
- Kidney infections
- Glomerulonephritis: Inflammation of the kidneys.
- Autosomal dominant polycystic kidney disease: An inherited condition characterized by the development of cysts in the kidneys.
- Urinary flow blockages: These can result from issues like recurring kidney stones or an enlarged prostate.
- Prolonged and regular use of specific medications, such as lithium and non-steroidal anti-inflammatory drugs (NSAIDs).
How is chronic kidney disease diagnosed and treated?
CKD is typically diagnosed through blood and urine tests, often as part of a routine check-up for people at risk of developing it. Once diagnosed, the doctor will determine the stage of CKD by measuring the level of creatinine, a waste product that accumulates in kidney disease. This measurement is called the estimated glomerular filtration rate (e-GFR) and reflects how efficiently the kidneys are cleansing blood.
CKD varies in severity and usually worsens over time, but early detection and treatment can slow its progression. Even if one kidney stops working due to this condition, the other may continue to function normally. Managing the risk factors can be achieved through annual tests, lifestyle changes, prescribed medications, and regular contact with a healthcare team.
Conversely, severe kidney failure resulting from CKD is known as end-stage renal disease, wherein patients require either frequent dialysis or a kidney transplant to survive.
Is a kidney transplant the right treatment option?
A kidney transplant is often the preferred treatment for kidney failure, compared to a lifetime of dialysis to effectively address CKD. It not only enhances a patient's quality of life but also offers a reduced risk of death, fewer dietary restrictions, and lower treatment costs in contrast to frequent dialysis. Some people may also benefit from a preemptive kidney transplant, which is conducted before the need for dialysis arises.
Living-donor kidney transplantation is an option since only one donated kidney is needed to replace two failed kidneys. If a compatible living donor is unavailable, the individual's name may be placed on a kidney transplant waiting list to receive a kidney from a deceased donor. Some individuals on the list may find a match within a few months, while others may wait several years.
However, for certain individuals with CKD, a kidney transplant may pose higher risks than dialysis. Factors that may disqualify someone from kidney transplant eligibility include advanced age, severe heart disease, recent cancer treatment, dementia, substance abuse issues, or any other condition that could impact the ability to safely undergo the procedure and adhere to post-transplant medications to prevent organ rejection.
How to prevent organ rejection?
Rejection is a significant risk following a transplant because the body may perceive the new kidney as foreign and attempt to attack it. To prevent rejection, it's crucial to adhere to the prescribed anti-rejection (immunosuppressant) medication regimen. These drugs suppress the immune system, reducing its response to the transplanted kidney.
Even if the patient feels well and believes the new kidney is functioning perfectly, they should never discontinue or miss their medication; since doing so can trigger rejection, which is often challenging to detect early and can result in permanent kidney loss.
What are the best practices after surgery for transplant success and recovery?
Recovery following kidney transplant surgery can vary from person to person. For some recipients, the new kidney may begin functioning immediately, while for others, it may take a few days, necessitating temporary dialysis until it becomes fully functional.
During the hospital stay, the individual will typically remain under observation for 3-4 days post-surgery, with close monitoring by the transplant team. It's common to experience some discomfort in the initial week after the procedure. Discomfort may manifest in the form of soreness in the abdominal and side areas, coupled with a sense of weakness and fatigue during the healing process.
Upon discharge, the patient will schedule follow-ups with their doctor, going in for appointments and laboratory tests 1-2 times per week at first. At home, the patient must maintain a vigilant focus on their health, monitoring their fluid intake, urine output, temperature, blood pressure and weight.
Most individuals typically achieve full recovery from the surgery within three months.
Key Takeaways
The kidneys play a vital role in maintaining our overall health, filtering waste, regulating blood pressure, and contributing to various essential bodily functions. However, chronic kidney disease (CKD) affects a significant portion of the global population, with up to 10% facing the gradual loss of kidney function due to various underlying factors like high blood pressure, diabetes, and infections, highlighting the importance of early diagnosis and management.
Depending on its stage, the treatment options for CKD range from lifestyle changes and medications to kidney transplantation. After a transplant, it's essential to strictly adhere to prescribed immunosuppressant medications, even if there are no apparent symptoms of rejection. Close monitoring during the hospital stays and consistent follow-ups with healthcare providers are essential. Full recovery typically occurs within three months post-transplant.
In the face of CKD, early detection, comprehensive care, and informed decisions regarding treatment options contribute to improved outcomes and a better quality of life.
Give it a "Like" and share your thoughts and questions with the community in the comments below!
Take care!
Sources:
Care after Kidney Transplant, National Kidney Foundation
Chronic Kidney Disease (CKD), American Kidney Fund
Chronic Kidney Disease (CKD), National Institute of Diabetes and Digestive and Kidney Diseases, NIH.org
Chronic Kidney Disease (CKD), Symptoms, causes, treatment, National Kidney Foundation
Chronic Kidney Disease (CKD), Kidney Care UK
Chronic Kidney Disease, NHS
Chronic Kidney Disease Basics, Chronic Kidney Disease Initiative, CDC
Chronic Kidney Disease, HealthDirect.gov.au
Chronic Kidney Disease, National Kidney Federation
Chronic Kidney Disease: Symptoms, stage, treatment, and more, Medical News Today
Epidemiology of chronic kidney disease: an update 2022, NIH.gov
Kidney Transplant, Johns Hopkins Medicine
Recovery after transplant surgery, American Kidney Fund
Stages of kidney disease, American Kidney Fund
Comments
You will also like
Kidney failure and transplantation: "My kidney is functioning perfectly after almost 10 years!"
Mar 11, 2021 • 3 comments

 Facebook
Facebook Twitter
Twitter