Dialysis: Everything you need to know!
Published Aug 27, 2021 • By Aurélien De Biagi
More than 661,000 Americans have kidney failure. Of them, 468,000 individuals are on dialysis. The discovery of dialysis techniques has revolutionized the management of patients with chronic kidney failure and has saved or prolonged hundreds of thousands of lives.
What is dialysis? What are the two types of dialysis? Which conditions may require dialysis?
We explain it all in our article!
What is dialysis?
Dialysis involves the elimination of waste from the body in a neutral liquid: dialysate. Physiologically in our body, the kidneys filter waste from the blood (about 180L of blood per day is filtered by the kidneys) and removes it through the urine. When the kidneys can no longer function, dialysis can be put in place to "replace" them. This is a technique which is part of renal replacement therapy (RRT) and provides only partial replacement of kidney function. The functions of hormone secretion and vitamin D processing cannot actually be substituted. Even so, dialysis allows the elimination of waste products not excreted by the kidneys as well as water that has built up in the body.
Depending on the dialysis technique used, the membrane may be biological (peritoneal dialysis) or synthetic (hemodialysis). The earlier it is started, the better the results.
What are the different types of dialysis?
There are two main types of dialysis: hemodialysis and peritoneal dialysis. In both cases, these are demanding techniques. Indeed, the patient must undergo dialysis sessions (4 to 5 hours per session and generally 3 sessions per week). In addition, the dialysis patient must follow a special diet which is low in salt, water, potassium and phosphorus.
Hemodialysis
This is the most common type of dialysis used. Hemodialysis consists of passing blood through an artificial membrane and then reinjecting it into the patient's body.
The equipment consists of a dialyzer which acts as a filter. It is made up of hollow synthetic fibers through which the blood circulates. Outside these fibers, the dialysate can circulate in counter-current to the blood, thus allowing an exchange between the two.
The hemodialysis machine forms dialysate: a liquid produced from purified water with a mineral composition similar to that of blood. The generator also allows the blood and dialysate to circulate in the dialyzer.
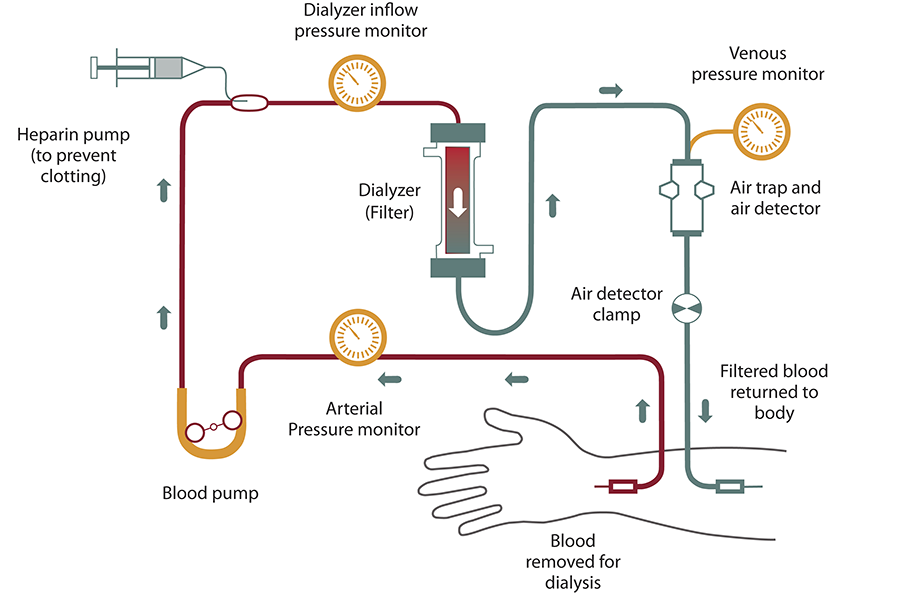
Source: NIH National Institute of Diabetes and Digestive and Kidney Diseases
Hemodialysis can be compatible with an active social and professional life; patients can adapt their dialysis schedule after discussion with their nephrologist.
Peritoneal dialysis
Peritoneal dialysis is the second possible type of dialysis. After 1-2 weeks of training, this form of dialysis can usually be performed by the patient themself or a third party.
Peritoneal dialysis uses the peritoneum as a filter. The peritoneum is a double layered membrane covering the organs and lining the inner surface of the abdomen. This method requires the surgical placement (under local or general anesthesia) of a catheter to create a peritoneal access. The catheter is fixed in the abdomen so that it does not move or interfere with the patient's movements and allows the dialysate to be introduced. In addition, once placed, the catheter is completely painless. The peritoneal cavity, which can hold up to four liters of dialysate, will be saturated within a few hours. This is why it is important to renew the fluid in the cavity.
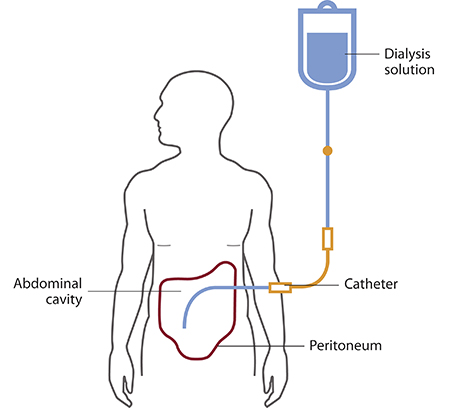
Source: NIH National Institute of Diabetes and Digestive and Kidney Diseases
This renewal can be done in different ways and patients can chose the type of peritoneal dialysis that best fits their lifestyle and schedule:
- Continuous ambulatory peritoneal dialysis (CAPD): Performed manually, 4-5 times daily. These exchanges normally take 30-40 minutes to complete.
- Automated peritoneal dialysis (APD): A machine, called a cycler, fills and empties the abdomen with dialysate 3-5 times during the night. In the morning, the patient starts the day with fresh solution in their belly and either leave the solution all day or perform one exchange in the afternoon without the machine. This is also sometimes called cycler-assisted peritoneal dialysis (CCPD)
Both CAPD and APD can be done in any clean, private, place - at home, at work, or when travelling. The two methods both also allow patients to exercise normally (though care must be taken with swimming) and to have an active socio-professional life by adapting the dialysate exchange schedule.
The choice of dialysis method is based on the patient's desire for autonomy, his or her self-image and lifestyle. Indeed, it is rarely based on purely medical issues. The only contraindications to hemodialysis are vascular disorders such as low blood pressure, diabetes and obesity. Those for peritoneal dialysis are severe obesity, a history of abdominal surgery complications, recurrent abdominal hernias and lack of diuresis (excretion of urine).
When is dialysis used?
Dialysis is used when the kidneys can no longer perform their physiological functions. For example, it is used when the kidneys can no longer filter during end-stage kidney failure. The causes of kidney failure can be numerous. Indeed, conditions such as high blood pressure and diabetes are the two main causes of chronic kidney failure.
The leading cause of dialysis in developed countries is diabetic nephropathy. Hyperglycemia due to diabetes damages the small vessels of the kidneys, leading to kidney dysfunction.
The second most common cause of end-stage renal failure is hypertension (high blood pressure). Indeed, it is associated with a narrowing of the small renal arteries and thus a reduction in renal vascularization.
Finally, other kidney diseases such as pyelonephritis (kidney infection), polycystic kidney disease and primary glomerulonephritis can lead to end-stage renal failure.
Was this article helpful to you?
Give it a like and share your thoughts and questions with the community in the comments below!
Take care!
Sources:
- Kidney Disease Statistics for the United States, NIH National Institute of Diabetes and Digestive and Kidney Diseases
- Hemodialysis, NIH National Institute of Diabetes and Digestive and Kidney Diseases
- Peritoneal Dialysis, NIH National Institute of Diabetes and Digestive and Kidney Diseases
- Insuffisance rénale, INSERM
- Comprendre la maladie rénale chronique, Ameli
- Le diagnostic et les traitements de l'insuffisance rénale chronique, Vidal
Comments
You will also like
Kidney failure and transplantation: "My kidney is functioning perfectly after almost 10 years!"
Mar 11, 2021 • 3 comments

 Facebook
Facebook Twitter
Twitter