Kidney Disease and the Coronavirus
Published Apr 28, 2020 • By Camille Dauvergne
Kidney disease is far from being a rare condition, with an estimated 37 million people affected by chronic kidney disease in the US. Kidney disease can lead to a gradual and irreversible deterioration in the kidneys' ability to filter blood and excrete certain hormones, known as renal failure. When renal failure is terminal, dialysis (a medical technique that cleans the blood) or a kidney transplant is required.
In the context of the COVID-19 pandemic, the CDC has indicated that patients with chronic kidney disease being treated with dialysis and those who have undergone an organ transplant are to be considered at higher risk for severe illness.
Is the risk the same for all kidney diseases? Do the treatments make you more susceptible to the virus? What precautions should you take when going for dialysis or to the hospital? Let us answer your questions!

I have renal failure and I've tested positive for COVID-19, is there a risk of complications?
Right now, more than 661,000 Americans have kidney failure. According to Professor Arnaud Méjean, urological surgeon at the Georges Pompidou European Hospital in Paris, it is important to consider the stage of renal failure in order to define the risk of complications from COVID-19.
As a reminder, the severity of renal failure is determined by the Glomerular Filtration Rate (GFR) number, which is a measure of kidney function.
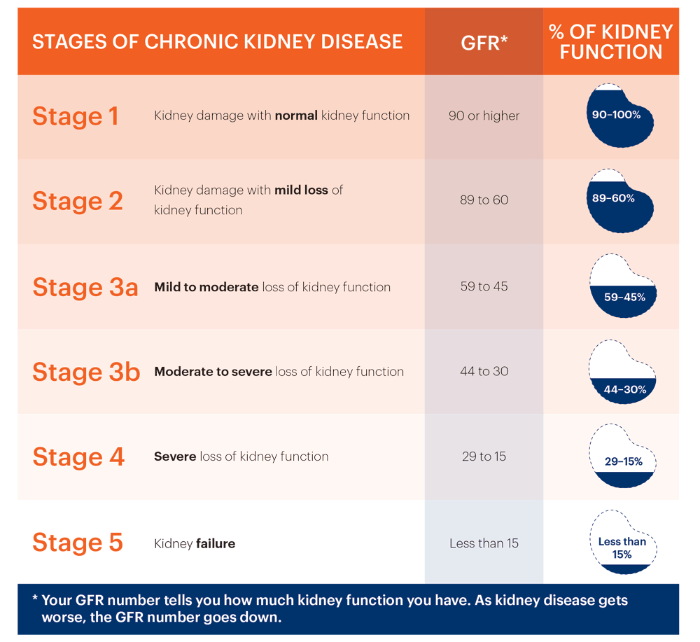
Source: The National Kidney Foundation
If your GFR is greater than 45, indicating that you have mild to moderate chronic kidney disease (CKD), the risk is no greater than in the general population.
However, according to Professor Méjean, the risk of complications is greatly increased if you have end-stage renal failure (<15 GFR) or are a transplant recipient and test positive for COVID-19.
In cases of dialysis, the risk is greater because of the patients' repeated exposure (several times a week) when travelling to and from the dialysis session as well as on site at the dialysis center. It is therefore important to implement the barrier gestures, to be able to identify the COVID-19 symptoms in order to alert your health care team in case of suspicion and to avoid refreshments and food during the sessions.
What are the risks in cases of acute renal failure?
The risk lies more in the care for patients than in the pathophysiology of renal failure. Professor Méjean, as well as many other doctors in the hospital and private sectors, are concerned about the fact that many patients who suffer from an acute illness (characterized by a sudden onset, rapid evolution over a short period of time), including acute renal failure, no longer go to the emergency room for fear of contracting COVID-19. These doctors fear an explosion acute illness complications due to a delay in the care of these patients after the coronavirus crisis.
Professor Méjean therefore reminds all patients that despite the risk of contracting COVID-19 in hospital, no condition should be left untreated! Patients should continue to consult their GP or specialist and visit hospital or treatment center for their chronic illness and in case of acute complications unless otherwise advised by medical staff. If there is an emergency, be it for COVID-19 symptoms or any other symptom, you should call 911!
Do my kidney treatments make me more susceptible to the virus?
Treatments for kidney failure are treatments for the condition that caused the kidney failure. About 50% of cases of severe kidney failure is due to diabetes or high blood pressure, but there are other factors such as the progression of complicated pyelonephritis, polycystic kidney disease or other degenerative diseases.
If you have any comorbidities (conditions associated with your kidney failure) such as diabetes or high blood pressure, which are risk factors for developing a severe form of COVID-19, it is especially important to take your regular course of treatment to keep them stable. Under no circumstances should you stop or change your treatments without the advice of your treating physician, as this may destabilize your condition without protecting you from complications of IDVOC-19.
Therefore, it is not the treatments that make you more sensitive to the virus, but the comorbidities when they are not properly stabilized by treatment.
Why is the risk greater if I am a transplant recipient and on anti-rejection medications?
Approximately 3,000 kidney transplants take place each year in the UK. When you have a kidney transplant, it becomes necessary to take a lifelong immunosuppressive (anti-rejection) medication, such as NEORAL, PROGRAF, ADVAGRAF, or AZATHIOPRINE. These are often combined with corticosteroids such as Prednisolone. These medications prevent transplant rejection by lowering your immune system response. You are therefore more weakened on an immune level while on these medications than without, which makes you more vulnerable to infection. This exposes you to a greater risk of developing complications following a SARS-CoV-2 (coronavirus) infection.
Although observance of the barrier gestures is naturally recommended in the case of a transplant, it is all the more encouraged in today's context, and strict confinement should be respected for your protection.
Why has my kidney transplant surgery been cancelled? Isn't this an emergency?
CDC and CMS has stated that transplants are going ahead if it is safe and appropriate, but transplant centers are assessing individual cases and the situation in their own hospital. Some centers may still need to look at temporarily putting elective living donor transplantation or non-urgent deceased donor transplants on hold. Again, decisions are being made on a case-by-case basis, taking into account issues such as the level of circulating COVID-19 infection in their areas and/or operational issues (such as testing availability, bed space, availability of basic supplies and equipment, including personal protective equipment).
Professor Méjean explains that it is possible to postpone a kidney transplant procedure thanks to dialysis. In fact, more than 50% of patients with end-stage renal failure are treated by dialysis and 45% undergo a transplant. Therefore, more than half of patients with end-stage renal failure are treated by dialysis, which provides effective management.
There are two types of dialysis:
- Hemodialysis: normally done three times a week for a four hour period, this treatment purifies the blood through a filter and is performed in a dialysis unit.
- Peritoneal dialysis: a treatment that uses the lining of your abdomen, called your peritoneum, and a cleaning solution called dialysate to clean your blood. This can be done at home.
The cancellation or postponement of a surgical operation due to COVID-19 is an informed and justified collective decision, which aims to free up hospital places for the emergency management. All procedures considered urgent and vital by your medical team are upheld.
How can I carry out my medical follow-up when hospital visits are strongly discouraged?
Very often, the hospital will keep you informed of the measures to be put in place for your follow-up.
If the consultation at the hospital was deemed avoidable by the care team, you will be contacted beforehand to prepare for a Telehealth or other sort of consultation. On the day of your visit, the department doctor will call you to review your clinical situation, your check-up and your treatment. A new prescription will be sent to you and a new consultation date will then be proposed.
If the consultation at the hospital was deemed necessary, no one will contact you beforehand and you will be able to go to your scheduled appointment as usual. Hospitals have put in place barrier gestures for arriving patients.
For dialysis patients who have to go to dialysis centers several times a week (more than 90% of dialysis patients), specific measures have been put in place to ensure optimal protection.
How do I protect myself?
Patients undergoing dialysis and kidney transplants must respect the barrier gestures, both in times of health crisis and in normal circumstances, as they are weakened and potentially permanently exposed to a multitude of viruses, bacteria and fungi. Self-isolation should be as stringent as possible, and contact with people who regularly go outdoors should be kept to a minimum.
Those at high risk, such as transplant patients and chronic kidney disease patients, are advised to continue sheltering in place until your state or region has entered Phase Three of the Opening Up America Again Guidelines.
Many patients feel anxious about the risk of developing complications with COVID-19 due to their current state of health, about the lack of protective equipment like masks, about possible changes in their medical care, etc. It is important for you to continue your regular treatment, to consult your doctor regularly and to respect the isolation and the barrier gestures as much as possible.
In order to best answer the questions and concerns of people affected by kidney disease, organ donation or transplantation and their families, the National Kidney Foundation provides a phone support service in English and Spanish. Call toll-free at 1.855.NKF.CARES (1.855.653.2273) Monday - Friday from 9:00 am - 5:00 pm ET or email here.
Was this article helpful to you? Do you have any other tips to share with the community?
Take care and stay safe at home!
Sources :
https://www.francerein.org/region/pays-de-la-loire/actualite/15-quelques-chiffres-cles
https://www.france-assos-sante.org/2020/04/06/activite-greffes-ralentie-covid-19/
https://www.inserm.fr/information-en-sante/dossiers-information/insuffisance-renale
https://www.sfndt.org/actualites/recommandations-covid-19
Comments
You will also like

Kidney failure and transplantation: "My kidney is functioning perfectly after almost 10 years!"
Mar 11, 2021 • 3 comments

 Facebook
Facebook Twitter
Twitter

