Monkeypox: everything there is to know!
Published Aug 12, 2022 • By Claudia Lima
Monkeypox is an infectious viral disease.
Monkeypox epidemic is affecting a growing number of countries, which is why on 23 July, 2022, the WHO declared monkeypox an international health emergency. This declaration will trigger a series of actions by member countries.
But what exactly is monkeypox? Where does it come from? What are its symptoms and how can the disease be treated?
Find all the answers in our article!
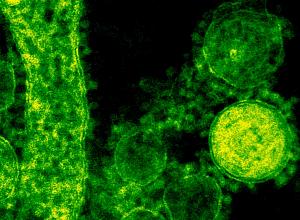
Monkeypox, also called simian pox or poxvirus, is a viral disease.
The name monkeypox is debatable because the disease is not specifically related to monkeys. The WHO has even been thinking of changing the name.
Monkeypox is a type of virus that uses humans as a natural host. It is related to the smallpox virus.
Key information about monkeypox
According to cdc.gov, there are more than 10,000 confirmed cases of monkeypox in the US. The most affected states are New York, California and Florida.
Today, more than 20,000 cases have been confirmed worldwide, with 79 deaths at the beginning of August 2022, including 4 outside Africa (2 in Spain, 1 in Brazil and 1 in India). Little information is available about the profile of the deceased.
Where does monkeypox come from?
Monkeypox is a disease caused by a virus that is transmitted to humans by animals (a viral zoonosis). It is usually transmitted by rodents or primates. The virus can then circulate among humans.
It is usually found in West or Central Africa, near tropical rainforests and increasingly in urban areas.
Monkeypox was first identified in humans in 1970 in Africa. In 2003, the first outbreak of monkeypox outside of Africa occurred in the United States of America. In May 2022, several cases of monkeypox were reported in non-endemic countries.
What are the symptoms of monkeypox?
The symptoms of monkeypox may begin with:
- Fever,
- Headache,
- Sore throat,
- Muscle pain,
- Lymphadenopathy or swollen lymph nodes,
- Rash, which appears a few days after the fever, and is located mainly on the face, palms and soles, ano-genital area, and also on the trunk and limbs,
- Itching.
The skin rash caused by monkeypox evolves from macules (flat-based lesions) to papules (raised lesions) and then vesicles (fluid-filled lesions) that progress to dryness and become pustules, which end up as crusts when they heal, and eventually fall off.
The evolution of this type of the disease is generally benign, monkeypox heals in 2 to 4 weeks. The incubation period can vary from 5 to 21 days. The fever lasts about 1 to 3 days.
Complications occur in 1-10% of cases, however, monkeypox is more severe in children, pregnant women and immunocompromized individuals.
Complications may arise from secondary infection of skin lesions or from respiratory, digestive, ophthalmologic, or neurologic damage.
It is recommended not to scratch the lesions, and to cover them, in order to reduce the risks of infection.
How is monkeypox diagnosed?
In order to establish the diagnosis, the doctor will have to make a differential diagnosis and eliminate other rash diseases such as chickenpox, shingles, measles, etc.
To confirm the diagnosis, a laboratory test, PCR (polymerase chain reaction), is necessary: it is a molecular biology technique identical to that used for the detection of the Covid-19 virus. The specimen is preferably taken from skin lesions; biopsy is also an option and the samples can be taken by rubbing several vesicles; lesion samples can also be collected from the nose and throat if the person has a rash in the mouth or throat.
How is monkeypox transmitted?
A person infected with monkeypox is contagious once the symptoms appear, which means that as long as there are no symptoms, there is no risk of transmission. However, once the disease has broken out, the infected person is contagious until the lesions have completely healed.
The virus can be transmitted by direct contact with the skin lesions or mucous membranes of an infected person, as well as by droplets (saliva, sneezing, sputum). Sexual intercourse, with or without penetration, meets the conditions for contamination. It can also occur through contact with the infected person's environment, like bedding, towels, clothing, etc. It is therefore important for patients to remain isolated throughout the duration of the disease and until the last crusts have disappeared.
In case of contamination by the virus, isolation of the sick person and the application of barrier measures is essential. Contact with domestic animals should also be avoided, as the risks of transmission and retransmission to humans are high.
How to avoid being contaminated with monkeypox?
Monkeypox can affect anyone.
Given what has been observed in the countries with high incidence, it would seem that cases are more numerous among MSM, an acronym that refers to all men who have sex with men, regardless of whether they identify themselves as heterosexual, bisexual or homosexual.
Thus, targeted communication campaigns were quickly implemented, including a digital campaign, a poster campaign, a broadcast of radio commercials and also the distribution of advice flyers.
A digital campaign on preventive vaccination started on 25 July 2022.
The French Health Body recommends preventive vaccination for: MSM, trans people with multiple sexual partners, professionals working in sexual consumption venues, male and female sex workers.
Preventive vaccination for healthcare professionals is considered on a case-by-case basis, depending on the degree of the exposure to the virus, on the existence of individual risk factors or at the direct request of the person concerned.
The recommended vaccination is:
- Two doses in post-exposure, i.e. for people in risky contact with an infected person,
- A single dose for people who were vaccinated against smallpox during their childhood, i.e. before 1980,
- Three doses for immunocompromized people.
The vaccine's name in the US is Jynneos®, it is known as a 3rd generation vaccine, which means it has been improved to induce fewer side effects.
Vaccination does not provide immediate protection.
Simultaneous administration of the vaccine with other vaccines such as Covid-19, or with drugs or immunoglobulin infusion has not been studied.
Vaccines are effective in preventing infection with monkeypox and severe course of the disease even several days after exposure to the virus.
How is monkeypox treated?
Proper management of the disease greatly reduces the risk of complications from monkeypox. Most people recover spontaneously.
In general, only symptomatic treatment is needed, for example, to reduce the fever (paracetamol) and calm the itching. The use of non-steroidal anti-inflammatory drugs (NSAIDs) is contraindicated as they may provoke severe forms of infection.
To prevent scratching of the skin, secondary infection of lesions and transmission of the virus, antihistamines can be prescribed, and it is advisable to cover the lesions.
For the most fragile people, an antiviral treatment (tecovirimat) or immunoglobulins can be prescribed by an infectiologist.
Some countries have implemented certain rules restricting the importation of rodents and primates, the main transmitters of orthopoxvirus.
Normally, this virus is difficult to transmit from human to human, except in the case of close and prolonged contact between two people. However, human-to-human transmission seems to be more present than expected and thus raises questions. Studies are underway to learn more about the increase in human-to-human transmission, particularly through respiratory droplets which may play a role in the transmission of the disease. Other studies show that this transmission pattern is probably due to the worldwide decline in immunity to viruses of the orthopoxvirus genus following the end of smallpox vaccination in the 1980s.
Sources :
Epidémie de Monkeypox - Variole du singe, qui est concerné et comment se faire vacciner ?, Service-public.fr
Variole du singe - vaccination-info-service.fr
Monkeypox, SantéPublique.fr
Un point sur la variole du singe, Inserm.fr
Variole du singe, conseils et prise en charge en Île-de-France, Ars.Sante.fr
Traitement de la variole du singe, ameli.fr
Principaux repères sur l'orthopoxvirose simienne, who.int.fr
Variole du singe, le potentiel épidémique augmente tant que l'immunité diminue, pasteur.fr
1 comment
You will also like

What are the dangers associated with the over-the-counter sale of certain medicines?
Dec 19, 2020 • 6 comments

 Facebook
Facebook Twitter
Twitter